A structured clinical approach for dealing with these sometimes horrific injuries
The treatment of facial burns is probably one of the most controversial subjects in plastic surgery today. There is no consensus among the leading burn institutions regarding the type of treatment, the timing of surgical intervention, the technique to be used, or the follow-up care, as shown during a symposium at the most recent meeting of the American Burn Association.1 This article is intended to be a structured overview of available treatment options with some recommendations based on my personal experience.
Almost all flame-caused burn injuries involve the face to some degree. Whereas most other scars on the body can be hidden with reasonable effort, facial-burn scars are obvious at first sight. Therefore, facial-scar prevention must be one of the main objectives when burn patients are treated.
There are some obstacles to overcome, especially in the case of large-surface-area burns, when survival and wound closure are at stake. The excision and grafting of a deep facial burn is blood-product- and donor-site-intensive.
Second-Degree Facial Burns
The typical conservative approach to second-degree facial burns includes topical ointments, such as antimicrobials, and enzymatic debridement agents, such as collagenase, which are usually applied until the wound has healed.2–4 If there are remaining open wounds after 3 weeks, or whenever the patient is stable, a split-thickness unmeshed skin graft is usually applied according to the “aesthetic unit principle.”5 After the wound has healed, various pressure treatments (described below) are implemented as deemed necessary.

Certain skin types (Fitzpatrick types III and IV) and age groups (small children and male teenagers) seem to be predisposed to hypertrophic scarring, moreso with dermal injury than with deeper burns.6,7 Delaying treatment of a deep dermal burn can lead to infection and, ultimately, the loss of underlying cartilaginous structures.8
Pressure- and silicone-therapy modalities often do not work well in the most mobile areas of the face, such as the perioral and periorbital regions. Yet, those areas are the most prone to the development of contractures. Microstomia and ectropion are a common occurrence after deep-dermal and full-thickness facial burns.
For children, wearing a face mask—whether flexible or clear plastic—to school can have a major psychological impact. The spontaneous healing of a second-degree deep dermal burn in the bearded area of the male face regularly leads to sebaceous inclusion cysts that are very cumbersome to treat and imply an additional social stigma.
Clinical trials have been performed to investigate a more aggressive approach to addressing these problems.9–11 All of these studies include this treatment: the aggressive debridement of sloughed skin, at the bedside or in the operating room, and immediate coverage with an adherent wound dressing such as a synthetic skin substitute, allograft, xenograft, amniotic membrane, or petroleum jelly gauze.
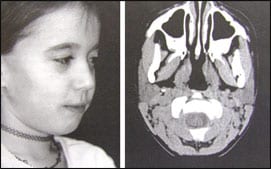
In the next step of this more aggressive approach, growth factors are introduced into the dressing via allogenic cells (such as cultured fibroblast cells or allogenic keratinocytes).12 An even more aggressive approach is to completely remove all necrotic cells and tissues by dermabrasion before applying a temporary growth-factor-laden matrix dressing (Figure 1).13–16
Indications for Dermabrasion
Although only the epidermis sloughs off in second-degree-burn wounds—which is related to the “natural” separation at this skin level with blister formation—the definition of second-degree burns implies that the heat damage reaches anywhere from the basal membrane to just above the subcutaneous tissue. Although widely used, the first-, second-, and third-degree burn classification is based on a purely anatomical definition, and it is really not feasible in modern burn-care practice.

Unfortunately, no objective measurement exists that will predict whether a dermal burn will heal from within. The wound’s appearance changes, not only within the first 48 hours, but also after the application of various wound dressings and creams. Furthermore, in a body area without hair growth—such as the forehead; upper inner arm and thigh; or back of the ear, ankle, or wrist—a given anatomical depth of a burn may not heal, whereas it would heal sufficiently in a hairy body area such as the outer forearm or the bearded portion of the face.

This more aggressive treatment eliminates some psychosocial implications of the conservative approach, such as the pain experienced during dressing changes and the inconvenience of ointment application every 2–4 hours to prevent the wound from drying and causing a deeper injury. Scar formation also appears to improve with more aggressive treatment, but no formal study has been done to prove this.
Third-Degree Facial Burns
In a deep facial burn with cartilage and subcutaneous tissue damage, the conservative approach consists of applying topical ointments for varying durations (periods of 24 hours to 3 weeks have been suggested), followed by excision and split-thickness grafting. In clinical practice, most deep facial burns occur in conjunction with a burn over a large area of the body, with or without inhalation injury. These contributing factors greatly limit the ability to stabilize the patient for a meticulous 3–4-hour excision within the first 3–5 days.

Any surgeon who has followed patients for several years after surgery knows what a poor solution this “standard-of-care” approach is to deep facial burns. The “aesthetic units” look like a mask, even years after the scars have matured, and no amount of reconstructive surgery can change their appearance.
Recently, the use of a dermal template has enabled us to achieve a more uniform appearance with more flexibility of the scar.21,22 In this approach, the excision is timed as early as possible and, in my experience, better results are achieved if the dermal-regeneration template is applied after an intermediate step with a xenograft or an allograft for hemostasis.
At the time the dermal-regeneration template is applied, the periorbital area is covered with a full-thickness graft, if available, and a tarsorrhaphy is performed.23 After the template matures (2–4 weeks), the silicone layer is removed and a split-thickness graft is applied in the largest single pieces possible—disregarding the “aesthetic units” principle.

In a newer approach, pre-expanded free flaps are used to reconstruct deep facial burns. This technique relies on the availability of normal skin that overlies a free-flap-suitable area such as the groin or the parascapular area.24,25
The newest development in the treatment of full-thickness facial burns is an allogenic full-face transplant. This endeavor is in preparation at some major teaching institutions. (See pages 40–42 in this issue—Ed.)
Scar Treatment
After wound healing is complete and the degree of expected scarring has been assessed, various scar treatments can be implemented. The standard of care includes pressure treatments, silicone face masks, and silicone sheeting; followed by reconstructive procedures in the areas of scar contracture, such as eyelid releases, mouth-angle releases, and nose reconstructions; and steroid injections into the most hypertrophic areas.26–31
In addition to the standard scar-treatment modalities, several others are available that are not used as often. Salicylic acid and verapamil, applied in a cream base, are absorbed into the scar and decrease the inflammatory response and the formation of collagen.32–36 Their absorption can be optimized by applying a hydrogel or silicone sheet over the scar for 8 hours at night (Figure 4).

The entire field of scar treatment has not been well-explored. Additional new but costly interventions are currently under investigation.38,39
Our ultimate goal in burn care needs to be freedom from pain and scarless wound healing, but currently there are many individual limitations to the delivery of even the standard care today. The knowledge of available alternatives and continued research into the underlying physiology of wound healing and scar formation will move us closer to our goal. PSP
Sigrid Blome-Eberwein, MD, is a board-certified plastic surgeon at the Lehigh Valley Regional Burn Center, Lehigh Valley Hospital, Allentown, Pa. She can be reached at (484) 695-7338 or [email protected]
References
1. Donelan MB, Sheridan RL, Spence RJ. Comprehensive management of facial burns. Paper presented at: Annual Meeting of the American Burn Association; May 10–13, 2005; Chicago, Ill.
2. Fraulin FO, Illmayer SJ, Tredget EE. Assessment of cosmetic and functional results of conservative versus surgical management of facial burns. J Burn Care Rehabil. 1996;17:19–29.
3. Heimbach DM, Engrav LH, Marvin J. Minor burns: Guidelines for successful outpatient management. Postgrad Med. 1981;69:22–26, 28–32.
4. Demling RH, DeSanti L. Management of partial thickness facial burns (comparison of topical antibiotics and bio-engineered skin substitutes). Burns. 1999;25:256–261.
5. Converse JM. Reconstructive Plastic Surgery. Philadelphia, Pa: WB Saunders; 1977.
6. Hunt JL, Purdue GF, Spicer T, Bennett G, Range S. Face burn reconstruction—Does early excision and autografting improve aesthetic appearance? Burns Incl Therm Inj. 1987;13:39–44.
7. Holmes JD, Muir IF, Rayner CR. A hypothesis of the healing of deep dermal burns and the significance for treatment. Br J Surg. 1983;70: 611–613.
8. Bentrem DJ, Bill TJ, Himel HN, Edlich RF. Chondritis of the ear: A late sequela of deep partial thickness burns of the face. J Emerg Med. 1996; 14:469–471.
9. Jonsson CE, Dalsgaard CJ. Early excision and skin grafting of selected burns of the face and neck. Plast Reconstr Surg. 1991;88:83–92; discussion 93–94.
10. Cole JK, Engrav LH, Heimbach DM, et al. Early excision and grafting of face and neck burns in patients over 20 years. Plast Reconstr Surg. 2002;109: 1266–1273.
11. Jonsson CE. The surgical treatment of acute facial burns. Scand J Plast Reconstr Surg Hand Surg. 1987;21:235–236.
12. Matouskova E, Broz L, Pokorna E, Konigova R. Prevention of burn wound conversion by allogeneic keratinocytes cultured on acellular xenodermis. Cell Tissue Bank. 2002;3:29–35.
13. Barkau M. Comparative study of 284 abraded and nonabraded burns [in French]. Acta Chir Belg. 1964;63:902–933.
14. nii-Amon-Kotei D, Thielen RG, Hofmann-von-herr S, Pieper WM. Abrasion method for the immediate management of surface thermal injuries of childhood. Z Kinderchir Grenzgeb. 1980;29: 283–291.
15. Lorthioir J. Burns. II. The abrasion treatment of burns. Mod Trends Plast Surg. 1964;16:89–95.
16. Serafini G. Treatment of burn scars of the face by dermabrasion and skin grafts. Br J Plast Surg. 1962;15:308–313.
17. De Souza BA, Furniss D, Jawad M. The use of sandpaper as a precision tool for dermabrasion in burn surgery. Plast Reconstr Surg. 2005;116: 350–351.
18. Stegman SJ. A comparative histologic study of the effects of three peeling agents and dermabrasion on normal and sundamaged skin. Aesthetic Plast Surg. 1982;6:123–135.
19. Suo JX. Autodermabrader in the early operation for deep second degree burns. A new operative mode in burns [in Chinese]. Zhonghua Wai Ke Za Zhi. 1992;30: 276–277, 317.
20. Engrav LH, Heimbach DM, Walkinshaw MD, Marvin JA. Excision of burns of the face. Plast Reconstr Surg. 1986;77:744–751.
21. Klein MB, Engrav LH, Holmes JH, et al. Management of facial burns with a collagen/glycosaminoglycan skin substitute—Prospective experience with 12 consecutive patients with large, deep facial burns. Burns. 2005;31:257–261.
22. Noah EM, Unglaub F, Ulrich D, Hartmann T, Pallua N. A case of successful delayed reconstruction using a collagen based dermal substitute of a chemical burn injury to the face caused by sulphuric acid. Burns. 2004;30: 280–282.
23. Frank DH, Wachtel T, Frank HA. The early treatment and reconstruction of eyelid burns. J Trauma. 1983;23:874–877.
24. Takushima A, Harii K, Asato H. Expanded latissimus dorsi free flap for the treatment of extensive post-burn neck contracture. J Reconstr Microsurg. 2002;18: 373–377.
25. Krastinova-Lolov D, Laxenaire A. The contribution of sliding skin flaps in the follow-up treatment of facial burns [in French]. Rev Stomatol Chir Maxillofac. 1997;98(suppl 1):124–128.
26. Williams F, Knapp D, Wallen M. Comparison of the characteristics and features of pressure garments used in the management of burn scars. Burns. 1998;24: 329–335.
27. Staley MJ, Richard RL. Use of pressure to treat hypertrophic burn scars. Adv Wound Care. 1997;10:44–46.
28. Gilman TH. Silicone sheet for treatment and prevention of hypertrophic scar: A new proposal for the mechanism of efficacy. Wound Repair Regen. 2003;11:235–236.
29. Kuhn MA, Moffit MR, Smith PD, et al. Silicone sheeting decreases fibroblast activity and downregulates TGFbeta2 in hypertrophic scar model. Int J Surg Investig. 2001;2:467–474.
30. Musgrave MA, Umraw N, Fish JS, Gomez M, Cartotto RC. The effect of silicone gel sheets on perfusion of hypertrophic burn scars. J Burn Care Rehabil. 2002;23:208–214.
31. Blaha J. Permanent sequelae after burns and tested procedures to influence them. Acta Chir Plast. 2001;43:119–131.
32. Danielson JR, Walter RJ. Salicylic acid may be useful in limiting scar formation. Plast Reconstr Surg. 2004;114:1359–1361.
33. Berman B, Villa AM, Ramirez CC. Novel opportunities in the treatment and prevention of scarring. J Cutan Med Surg. 2004;8(suppl 3):32–36.
34. Skaria AM. Prevention and treatment of keloids with intralesional verapamil. Dermatology. 2004; 209:71.
35. Wang Z, Guo S, Lu K. The biological effect of verapamil on hypertrophic scar fibroblast [in Chinese]. Zhonghua Zheng Xing Wai Ke Za Zhi. 2001; 17: 328–331.
36. Doong H, Dissanayake S, Gowrishankar TR, LaBarbera MC, Lee RC. The 1996 Lindberg Award. Calcium antagonists alter cell shape and induce procollagenase synthesis in keloid and normal human dermal fibroblasts. J Burn Care Rehabil. 1996;17(pt 1):497–514.
37. Patino O, Novick C, Merlo A, Benaim F. Massage in hypertrophic scars. J Burn Care Rehabil. 1999; 20:268–271; discussion 267.
38. Eberlein A, Schepler H, Spilker G, Altmeyer P, Hartmann B. Erbium:YAG laser treatment of post-burn scars: Potentials and limitations. Burns. 2005; 31:15–24.
39. Kwon SD, Kye YC. Treatment of scars with a pulsed Er:YAG laser. J Cutan Laser Ther. 2000; 2:27–31.