Scalp defects secondary to illness and injury are relatively common. The challenges vary widely in severity, morphology, and etiology, and represent a formidable challenge not only to repair the anatomic defect but also to correct the residual cosmetic deficiencies. Most defects require a combination of cosmetic and reconstructive techniques to achieve the best results.
Hair transplantation is a key cosmetic surgery component in correcting these unique deformities; however, treating the extensive scalp-loss patients continues to be a significant challenge that cannot be addressed with hair transplantation. In addition, the implications of future hair loss due to androgenetic alopecia greatly affect surgical planning.
This article will focus on the challenge of major scalp defect reconstruction in achieving a cosmetically superior result.
INTRODUCTION
Hair loss may take many forms, including natural male and female pattern baldness, trauma, cancer, and iatrogenic causes. The treatment of naturally occurring hair loss has been refined over many decades. Contemporary hair restoration surgery (HRS) techniques are able to treat the vast majority of natural hair loss or Androgenetic Alopecia (AGA)—commonly known as male pattern hair loss. Illness or injury, however, often cause significant hair loss defects that cannot be adequately treated with current HRS techniques, so we have to reach into our reconstructive armamentarium for procedures suited to treat massive hair loss from devastating illness or injury.
The degree of deformity generally determines the treatment choice. Advancements in HRS in the past 2 decades are significant in yielding natural and almost undetectable results. Using a combination of HRS and cosmetic and reconstructive techniques, most deformities can be treated effectively. This article will give the reader an overview of HRS cosmetic and reconstructive options, and applications for their use in scalp reconstruction.
Effective scalp reconstruction requires understanding the basic concepts of HRS. HRS has become more complex as we have identified the important variables in achieving natural results, which include the natural history of hair loss (AGA), hairline design, recipient-site creation, and graft preparation. Also important is understanding the natural history of hair loss and modifying its course with contemporary medical therapy for hair loss.
ANDROGENETIC ALOPECIA
AGA is not strictly considered a scalp defect. However, the methods developed to treat AGA underlie the same techniques used for treating significant scalp deformities. After all, hair deformities are usually unsightly cosmetic problems. Therefore, understanding the development of cosmetic as well as reconstructive procedures are important aspects in treating these deformities.
Methods of treating all forms of hair deformities evolved from this early work and contribute to our abilities to treat many complicated problems today.
The exact mechanism of AGA is not clearly understood, but the presence of the male hormone dihydrotestosterone (DHT) is required for men with a genetic predisposition for baldness to demonstrate the trait. Hamilton, an anatomist,1 first recognized this relationship in 1942 while studying castrated men who did not develop AGA until exogenous testosterone was administered. Those who were genetically prone to AGA lost their hair correctly, deducing that testosterone is needed for phenotypic expression.
Even today, the exact mechanism has not been known. However, a major focus of current medical therapy is based on blocking the synthesis of DHT with finasteride.2,3
Another important FDA-approved medication that helps to slow or reverse AGA is minoxidil, which is a topical formulation applied to the scalp twice daily. The exact mechanism for its effect is unknown, but its efficacy in double-blinded placebo-controlled studies is significant. Unlike finasteride, minoxidil may be used by both men and women.
The HairMax Laser comb is a new device cleared by the FDA in 2007 to promote hair growth. More published experience with the device is expected in the near future.
Medical therapy should be considered in any HRS treatment as continued hair loss will slowly but surely “undo” any reconstruction procedure. Chronic treatment will slow, prevent, or even reverse the AGA process, making it an important tool in HRS.
HRS TECHNIQUES
With this as background, let us acknowledge that there are many HRS techniques today, including follicular unit transplantation (FUT is considered the gold standard), follicular unit extraction (FUE), scalp reduction, scalp flaps, and tissue expansion. This article will focus on repairing scalp deformities.
The alopecia reduction procedure was significant innovation first reported by Sparkuhl (1975), Blanchard,4 and Unger5 that allowed HRS surgeons to reduce or eliminate large amounts of bald scalp.
Larger reductions were made possible with the development of extensive scalp lifting,6 but with some increased risk of devascularization injury because of acute occipital ligation injury during the procedure.
Subsequently, Brandy advocated ligating the occipital artery as a “flap delay” 4 weeks prior to the scalping procedure.7 The author developed a procedure to preserve the occipital artery during scalp lifting that eliminated the need for preoperative ligation and virtually eliminated the risk for vascular compromise.8 Although challenging, this procedure has permitted the safe excision of large scalp scars.
Also critical in the evolution of treating scalp deformities is tissue expansion,9 which has found numerous applications in reconstructive surgery. Tissue expansion opens up the possibilities of excising large scalp deformities by safely creating more length in tissue, allowing the hair-bearing scalp to be reapproximated. The resulting scars are typically covered by hair, making tissue expansion an ideal procedure for treating many defects.
The range of scalp surgery has expanded considerably, creating a combination of innovations that allow the reliable treatment of many scalp deformities.
HAIR RECONSTRUCTION: UNDERSTANDING THE AESTHETIC ELEMENTS
The success of any HRS procedure depends upon many factors. Recognizing what is a normal-appearing hairline, though, is critical. The reader is directed to a complete discussion of this topic in Hair Transplantation, 4th edition.10 Natural cosmetic results are highly dependent on these factors, which include the following:
- Extent of hair loss or defect. This determines the amount of work required to cover the defect.
- Age of the patient. Bear in mind that the extent of hair loss increases with age. Young men with AGA will have less hair to transplant and more bald area to cover as they grow older. In scalp reconstruction, the balding process continues unabated and can have a significant impact on the future and longevity of the results.
- Adequate donor tissue (hair-bearing scalp). There must be sufficient donor hair density and tissue to provide enough grafts to cover the hair defect. Hair restoration does not produce more hair but, rather, relocates existing hair on the patient’s scalp.
- Hair color affects perceived coverage. The darker the color, the greater the apparent coverage per given hair density.
- Hair curl increases the apparent volume of hair present. Curly hair covers more area as it bunches up on itself.
- Hair contrast plays an important role in naturalness. The greater the contrast—for example, black hair on white skin—the more unnatural the appearance. Care must be taken to use the finest single hair grafts in the most exposed area; that is, the hairline especially after a reconstructive flap advancement.
- Hair shaft diameter is an important determinant in how much hair mass is moved. The thicker the diameter, the more prominent the hair and the more coverage it provides.
- Hair direction must be maintained to create a natural result. This element is critical and should be considered except in the most dire circumstance, where any coverage is acceptable.
- mHairline considerations. A natural hairline is a misnomer. A natural hairline is actually a zone of fine, irregular hairs that create the feathering zone as the bald scalp gradually yields to hair-bearing scalp.
- Ethnic differences are wide and varied, and usually can be described as a combination of the above characteristics. For example, Asian hair is less dense than Caucasian hair, but the hair shaft diameters are typically thicker. The converse is also true: Typically, Caucasians have greater density (hair follicles/mm2) but smaller shaft diameters.
HAIRLINE DESIGN
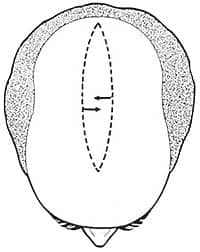
 |
| Figure 1. Original midline alopecia reduction pattern. |
Besides hair transplantation, scalp flap procedures are the mainstay of scalp reconstruction. While creating an undetectable and natural hairline often represents a great challenge to HRS surgeons, scalp flap techniques are able to cover large defects swiftly and effectively.
Alopecia reduction (AR) allows the surgeon to eliminate unwanted bald tissue. Originally innovated for cosmetic HRS in the 1970s, it is a procedure that became very popular because of its simplicity and effectiveness in reducing the amount of bald scalp requiring hair transplantation. Its popularity waned as hair transplantation techniques improved and our understanding of the natural history of hair loss became more refined. But the techniques remain valuable tools for reconstructive purposes.
The first AR procedures were simple excision of bald scalp from the central area of hair loss (Figure 1). Scalp was undermined to the nuchal line that is a prominent ridge on the parietal and occipital scalp where several muscle attach to the skull. Undermining in the subgaleal plane was easy, bloodless, and fast, allowing the surgeon to remove a significant area of bald scalp rapidly.
Limitations and disadvantages of AR were soon discovered including widening the bald area also known as stretch-back,11 slot deformity,12 and visible scarring. Many technique variations were developed to further improve the method to enhance bald scalp removal and minimize hair deformities.
The extensive scalp lift (ESL) is one of the more interesting and effective AR techniques in that the dissection was carried out beyond the limits of the galea aponeurotica marked by the nuchal line, extending it down to the nape of the hair-line.13 Furthermore, no expander devices were required. Brandy determined that the majority of the tissue stretch occurred in the tissue beyond the thick and less elastic galeal layer; thus, ESL permitted a much greater reduction of bald scalp.
 |
| Figure 2. This series of intraoperative photos demonstrates the technique and the effectiveness of the extensive scalp lift procedure, with preservation of the flap’s axial blood supply. |
This greater efficiency was not without greater complications, however, in that an incidence occipital hair-bearing scalp necrosis was noted. Mangubat developed the procedure to preserve the occipital artery of the posterior scalp and eliminated the incidence of necrosis (Figure 2).8
HAIR-BEARING FLAPS
Transposition of hair-bearing flaps was first reported by Juri,14 in which a long hair-bearing flap of scalp was transposed from the parieto-occipital scalp to the frontal hairline. Variations of this technique were developed with significant success by various authors.
Even though there were few complications, the avascular necrosis complications resulted in significant disfigurement, even in the best of hands. The subsequent loss of a considerable amount of donor hair is perhaps the greatest liability (Figure 5) and, as expected, the technique has been largely abandoned for elective cosmetic procedures used almost exclusively for scalp reconstruction.
TISSUE EXPANDERS
Tissue expansion is an extraordinary tool for repairing large skin defects. Prior to the tissue expansion techniques, repair of large skin defects was often ineffective. The history of the technique is similarly extraordinary in that it took more than 20 years to recognize its value to reconstructive work. The original work9 was not considered noteworthy, and its significance remained buried and unnoticed until another young surgeon demonstrated its usefulness in breast reconstruction.15 Its simplicity and popularity grew exponentially as industry became involved in producing commercially viable products.
 |
| Figure 3. Tissue expansion is completed in 10 weeks. The significant cosmetic deformity the patient must endure for 4 to 6 weeks is difficult for him to accept. |
The technique gradually expands a balloon implanted under the skin immediately adjacent to the defect via a series of percutaneous injections into a self-sealing filling port. As the balloon increases in size the tissue compensates by stretching, increasing its length and mass through mechanisms known as mechanical (stretching the collagen fibers) creep16 and biological (stimulating new tissue growth) creep.17
Mechanical creep is subject to shrinkage when the balloon is removed as the collagen fibers attempt to return to normal resting length. Biological creep, on the other hand, is not stretching in the traditional sense, as cellular actually increases the amount of tissue present. Both properties are critical to successful tissue expansion.
The use of tissue expansion in cosmetic procedures has been limited in part due to the significant deformity the patient must temporarily endure during the final stages of the process (Figure 3). Reconstructive patients, on the other hand, are more tolerant given the unsightly defects they are trying to repair.
Surgical planning is critical to successful tissue expansion. The patient and family must be counseled to expect a cosmetic deformity, especially near the end of the expansion process.
The size of the expander must be estimated preoperatively using one of several mathematical methods. It is best to overestimate needed expansion and choose the largest commercially available expander that fits the patient’s anatomy. In general, an expander with a base dimension roughly equal to the dimension of the defect that also has a large vertical expansion dimension is ideal. Most manufacturers have tables of expander specifications that ease the decision-making process.
 |
| Figure 4. Calipers can be used to measure the width of the expanded flap to be excised. The measured distance over the expanded flap minus the flap width yields the approximate distance of flap advancement. The actual yield is usually less than the measurement due to contraction of the collagen fibers (mechanical creep) and, thus, a 130% overexpansion is planned. |
The vertical dimension is the most important factor providing the greatest gain in flap expansion. When the distance over the expanded tissue minus the base width of the expander is equal to 120% of the width of the defect, the expansion is complete (Figure 4). Overexpansion by a modest amount will increase patient safety by providing an excess of tissue to cover the defect. Closing an expanded flap under tension could lead to flap necrosis. If complete excision is not easily accomplished, it is advisable to leave some residual defect, excise what is easily removed, and replace the same expander under the flap for a second expansion to proceed.
Generally, placement of the expander should be parallel to the longest side of the defect. This gives the greatest coverage. In hair-bearing scalp, paying attention to hair direction is important if the defect is adjacent to the hairline. In most cases, however, the hair can be trained to style appropriately.
Once expansion is completed and the measured distance over the expanded flap minus base width of expander is 120% of the width of the defect, the final flap advancement is executed.
Once the expander is removed, the flap advancement is tested to ensure the complete defect can be excised. If the entire defect cannot be removed, a blood stain is left on the distal portion of the defect that the flap can cover to mark the maximum tissue to be excised. Although the inability to close a defect with a fully expanded flap is not a common problem, the surgeon and patient must be prepared to accept the potential possibility. If the residual defect is significant, leave the expander in place for a second expansion.
CASE PRESENTATIONS
Scalp deformities secondary to trauma and cancer are challenging, The following examples demonstrate the utility of HRS techniques when added to cosmetic and reconstructive procedures in delivering excellent results when treating these difficult cases.
Case 1: Necrosis of hair flap (Figure 5)
Ten years ago, this 42-year-old male underwent bilateral superiorly based hair flap rotations in an attempt to reconstruct the hairline. The left flap necrosed and was replaced with a split-thickness skin graft, leaving him with a severe iatrogenic deformity. The most difficult part of this patient’s treatment was gaining his trust to perform a reconstruction. As a result, his treatment plan took several years.
The plan employed hair transplantation behind the scar, in a preliminary step to provide hair that would help cover the skin graft. Once the patient felt confident to continue, a pretrichial brow lift was performed to elevate the brow skin and excise the split-thickness skin graft. At the same time, the surviving flap on the right side was tailored to a more appropriate shape. The excised hair from the right flap was dissected into follicular units and added to the left hairline.
The significant improvement has motivated him to begin removing his hairpiece and expose his natural hair, and he plans more transplantation to fill the left side and complete the hairline.
 |
| Figure 5. Preoperative and postoperative views of a 42-year-old man disfigured by complete necrosis of superiorly based transposition flap. Multiple repairs were performed, including multiple hair transplants, brow lift, excision of skin graft, and refinement of surviving flap that required elevating the temporal hairline to a more acute angle using a brow lift and excision of excess hair-bearing scalp. The excised hair was “recycled” by creating hair grafts and placing them posteriorly. |
Case 2: Scalp defect from excision of skin neoplasm (Figure 6)
This 7-year-old boy was referred for HRS after having a large giant congenital nevus (at significant risk for developing neoplasm) excised as an infant. Now in grade school, he suffers teasing and he wishes to have the defect repaired.
Treatment was undertaken during summer vacation with a large tissue expander placed over the scalp vertex in such a position as to maximize movement of hair-bearing scalp. Before the end of the summer vacation, expansion was sufficient that complete excision of the defect was possible.
In Figure 6, note the hair direction is somewhat distorted but easily covered when the patient’s hair is longer. The future potential for AGA was discussed with the family. If he were to develop male pattern hair loss during his young adult life, more HRS would be required; however, for now his young life is free from teasing that could affect his social development.
 |
| Figure 6. An 8-year-old boy who had a nevus removed as an infant. The defect repaired with a skin graft (top left). Top right shows the completed expansion. Three months later, the scalp defect is closed (bottom photos). |
TRAUMA
Scalp burns are relatively common causes of hair deformities. Even a partial-thickness burn can destroy hair follicles and traumatic alopecia will result. Burns result in large, irregular scars, and tissue expansion is ideal for these difficult patients. Often, tissue expansion is prolonged because of scar rigidity, but despite the delay the expansion can be accomplished with little risk—as long as patient compliance is ensured.
Case 3: Large burn defect presenting after multiple failed treatment attempts (Figure 7).
This 35-year-old woman presented after having five prior procedures that attempted to repair a grease burn she suffered on her scalp as a child. The procedures included two scalp reductions and three hair transplants using 4-mm punch grafts.
She has had to wear her hair long in order to camouflage the defect. The scar and surrounding tissue is thick and rigid, allowing little, if any, movement that would permit excising the 25- x 8-cm defect.
Treatment consisted of placing a large, 1.3-L crescent-shaped expander in the occipital scalp directly adjacent to the defect. The extreme rigidity of the tissue required more than 9 months to complete expansion. The process was prolonged because of pain resulting from the excessive tissue rigidity. The result was particularly satisfying in that with two simple procedures the entire defect was closed.
 |
| Figure 7. Large defect left by a full-thickness burn as a child; multiple attempts at excision and hair transplants had not been successful. Expansion completed after 9 months due to rigid tissue. The expander is removed for trial advancement of the flap to ensure complete coverage of defect prior to excision. Complete excision of the large defect is performed. Last image shows immediate postop results. |
Case 4: Extensive scalp loss in a young boy (Figure 8).
This 8-year-old male was brought with a history of a local university plastic surgery department’s basically saying there was nothing more it could do for him. He was the victim of a house fire as an infant and suffered burns more than approximately 60% BSA.
Although he survived, he required numerous secondary procedures to manage his burns. Of particular interest were the multiple skin grafts required in the scalp. As he grew, his skull volume increased beyond the skin grafts’ elastic properties, causing graft necrosis. He then required annual skin grafting procedures throughout his young life. In addition, the more skin grafting he underwent, the greater the bald area he accumulated. The cosmetic appearance of a balding little boy in grade school caused much social turmoil.
He was almost in need of another skin graft when he presented to my clinic. This was a particular challenge in that he had lost more than 70% of his hair-bearing scalp. His calvarium was still young and pliable, making rapid tissue expansion more challenging to avoid skull deformities.
 |
| Figure 8. Views of thin skin grafts that will soon break down as the child grows. Unilateral and bilateral expansions complete to accommodate large bilateral scar excisions. Immediate postop results and 9 months postop showing the stretch back over time. Complete excision was not possible because of a cellulitis complication. The patient is still a work in progress. |
The treatment plan consisted of a two-staged expansion procedure. Because there is more hair-bearing skin in the right parietal scalp, it was expanded first. This eliminated a significant amount of the skin graft overstretched by the child’s growth. In addition, it gave me the opportunity to evaluate any significant skull deformity resulting from the tissue expander, as well as the child’s ability to cope with the expansion process.
Stage one was successful, which gave us the opportunity to proceed with bilateral scalp expansion.
Stage two proceeded a more slowly because the child developed a habit of picking at the skin overlying the expander port. Unfortunately, he developed a cellulitis that required hospitalization, IV antibiotics, and wound care before the expansion could be completed.
Following resolution of the cellulitis, it was clear that the child was not going to tolerate much more discomfort. With family input, we decided to take what we could get safely and delay any future procedures until he was mature enough to participate in his care. All of the skin grafting at risk for necrosis was replaced with expanded scalp and the scar was reduced more than 90%. With appropriate hairstyling, he is able to cover a significant portion of the disfiguring scar.
What lies in his future will depend on his maturity and what develops with his existing hair. As he approaches puberty, he may be subject to AGA although the majority of the scalp vertex most susceptible to AGA was burned in the fire; thus, we hope that AGA effects will be limited.
CONCLUSION
Contemporary HRS procedures can be combined with traditional reconstructive techniques to treat a wide spectrum of hair deformities. Specific education and training in HRS is not a traditional part of formal surgical training, although much information is available through several national and international organizations.
Your sensitivity to the unique variables associated with HRS will increase the chances of achieving a superior functional as well as cosmetic result when treating significant hair deformities. I continue to volunteer for Operation Restore, a pro bono program co-sponsored by the Hair Foundation and the International Society of Hair Restoration Surgery, which specializes in scalp reconstruction and provides free services for the ill and injured.
E. Antonio Mangubat, MD, is a board-certified cosmetic surgeon in Seattle. He can be reached at Southcenter Cosmetic Surgery at (206) 575-0300 or via e-mail at . More about Operation Restore can be found at www.ishrs.org/ishrs-pro-bono.
ADDITIONAL READING
- Nordstrom REA, ed. Tissue Expansion. Butterworth-Heinemann; 1996.
- Stough DB, Haber RS, eds. Hair Replacement: Surgical and Medical. Mosby; 1996.
- Unger W, Shapiro R, eds. Hair Transplantation. 4th ed. Marcel Dekker; 2004.
REFERENCES
- Hamilton JH. Male hormone stimulation is prerequisite and incitement in common baldness. Am J Anat. 1942;71:451.
- Kaufman KD. Androgen metabolism as it affects hair growth in androgenetic alopecia. Dermatol Clin. 1996;14(4):697-711.
- Price VH, Menefee E, Sanchez M, Ruane P, Kaufman KD. Changes in hair weight and hair count in men with androgenetic alopecia after treatment with finasteride, 1 mg, daily. J Am Acad Dermatol. 2002;46(4):517-523.
- Blanchard G, Blanchard B. Obliteration of alopecia by hair-lifting: a new concept and technique. J Natl Med Assoc. 1977;69(9):639-641.
- Unger MG, Unger WP. Management of alopecia of the scalp by a combination of excisions and transplantations. J Dermatol Surg Oncol. 1978;4(9):670-672.
- Brandy DA. The bilateral occipito-parietal flap. J Dermatol Surg Oncol. 1986;12(10):1062-1066.
- Brandy DA. The effectiveness of occipital artery ligations as a priming procedure for extensive scalp-lifting. J Dermatol Surg Oncol. 1991;17(12):946-949.
- Mangubat EA. Preservation of the occipital artery during extensive scalp lifting. Am J Cosmetic Surgery. 1997;14(2): 161-166.
- Neumman CG. The expansion of an area of skin by progressive distention of a subcutaneous balloon; use of the method for securing skin for subtotal reconstruction of the ear. Plast Reconstr Surg. 1957;19(2):124-130.
- Unger W, Shapiro R, eds. Hair Transplantation. 4th ed. Marcel Dekker; 2004.
- Nordstrom RE. “Stretch-back” in scalp reductions for male pattern baldness. Plast Reconstr Surg. 1984;73(3):422-426.
- Norwood OT, Shiell RC, Morrison ID. Complications of scalp reductions. J Dermatol Surg Oncol. 1983;9(10):828-835.
- Brandy DA. The bilateral occipito-parietal flap. J Dermatol Surg Oncol. 1986;12(10):1062-1066.
- Juri J. Use of parieto-occipital flaps in the surgical treatment of baldness. Plast Reconstr Surg. 1975;55(4):456-460.
- Radovan C. Reconstruction of the breast after mastectomy using a temporary expander. Plast Reconstr Surg. 1982;69:195-206.
- Mustoe TA, Bartell TH, Garner WL. Physical, biomechanical, histologic, and biochemical effects of rapid versus conventional tissue expansion. Plast Reconstr Surg. 1989;83(4):687-691.
- Van Rappard JH, Sonneveld GJ, Borghouts JM. Histologic changes in soft tissues due to tissue expansion (in animal studies and humans). Facial Plast Surg. 1988;5(4):280-286.
- Nordstrom REA, ed. Tissue Expansion. Butterworth-Heinemann; 1996:17.